Do Dry Sockets Heal On Their Own – Dry Socket Recovery!
Yes, dry sockets can heal on their own, but the process may be painful and prolonged without proper care.
This article explores the nature of dry sockets, their symptoms, treatment options, and whether they can heal on their own.
Do Dry Sockets Heal on Their Own?
Understanding Dry Sockets:

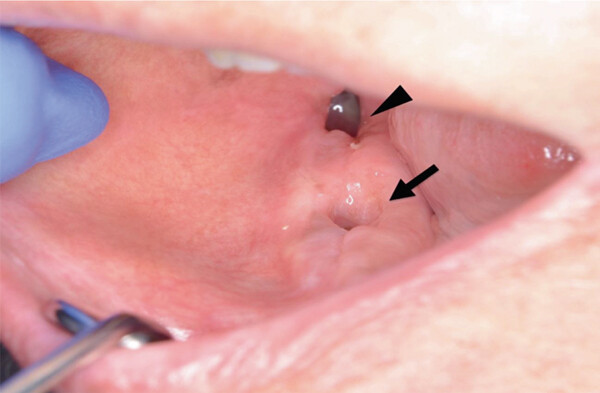
A dry socket, clinically known as alveolar osteitis, occurs when the blood clot that forms in the socket following a tooth extraction either becomes dislodged or dissolves prematurely. This clot is essential for protecting the underlying bone and nerve endings from exposure to air, food, and bacteria. The absence of this clot can lead to severe pain, increased sensitivity, and complications that can prolong the healing process. While many cases of dry sockets may resolve on their own, the journey to recovery can be painful and may require additional care.
How Dry Sockets Form?
Dry sockets typically arise several days post-extraction, commonly around the third to fifth day. Factors contributing to the development of a dry socket include:
- Dislodgment of the Blood Clot: Activities such as sucking on straws, vigorous rinsing, or even certain movements of the mouth can dislodge the clot.
- Infection: Bacterial contamination at the extraction site can dissolve the blood clot prematurely.
- Smoking: The suction from smoking can dislodge the blood clot, and the heat and toxins in tobacco can hinder healing.
- Oral Contraceptives: Women using oral contraceptives may be at a higher risk due to hormonal factors that affect blood clotting and healing.
- Previous History of Dry Sockets: Patients with a previous history of dry sockets may be more susceptible to developing them again.
- Trauma or Complicated Extractions: Surgical extractions or those involving significant manipulation of the bone can increase the likelihood of developing a dry socket.
Symptoms of a Dry Socket:
Recognizing the symptoms of a dry socket is crucial for timely intervention. Key indicators include:
- Severe Pain: Pain typically radiates from the extraction site to the ear, eye, temple, or neck on the same side as the extraction. This pain can begin suddenly and intensify over time.
- Empty Socket: Upon inspection, the extraction site may appear empty and have no visible blood clot. Instead, the bone may be exposed.
- Foul Odor or Taste: Patients may notice a bad taste or odor emanating from the extraction site, often indicative of food debris or infection.
- Swelling and Inflammation: Localized swelling may occur, and the surrounding gums can appear red and inflamed.
- Difficulty in Eating or Drinking: The pain can make it challenging to eat or drink comfortably, leading to potential nutritional deficiencies.
Also Read: How Long For Nose Piercing To Heal – A Comprehensive Overview!
The Healing Process of Dry Sockets:
While a dry socket can heal on its own, the process can be complicated. Healing generally involves the formation of new granulation tissue to cover the exposed bone. The timeframe for healing varies based on several factors:
- Severity of the Condition: More severe cases with significant exposure may take longer to heal. Mild cases might resolve within a week, while severe cases can linger for several weeks.
- Patient’s Overall Health: Factors such as age, nutritional status, and underlying health conditions (e.g., diabetes) can affect healing times. A healthy individual may experience a quicker resolution than someone with compromised health.
- Management of Symptoms: Effective pain management and care can support the healing process. Over-the-counter pain relievers like ibuprofen or acetaminophen can help alleviate discomfort, while prescription medications may be necessary for more severe pain.
Natural Healing and Its Implications:
Dry sockets can indeed heal without surgical intervention, but this process may be fraught with discomfort. As the body works to heal itself, patients may experience fluctuating pain levels. While the natural healing process is ongoing, it is essential to maintain good oral hygiene to prevent infection and facilitate recovery. This includes gentle rinsing with warm salt water, avoiding vigorous mouth movements, and refraining from irritating the extraction site.
When to Seek Professional ?
It is vital for patients to be vigilant about their symptoms following a tooth extraction. If any of the following occur, consulting a dental professional is recommended:
- Persistent or Worsening Pain: If pain does not improve after a few days or increases in intensity, it may indicate an unresolved issue.
- Signs of Infection: Symptoms such as fever, chills, or a foul-smelling discharge from the socket warrant immediate attention.
- Difficulty Managing Pain: If over-the-counter pain medications are ineffective, a dentist can prescribe stronger pain relief options.
- Visible Complications: If there are visible signs of infection or if the socket does not appear to be healing, further evaluation is necessary.
Dental Treatments for Dry Sockets:
If a dry socket is diagnosed, a dentist may implement various treatments to facilitate healing:
- Medicated Dressings: A dentist may place a medicated dressing within the socket to alleviate pain and protect the area. These dressings typically need to be changed regularly, often requiring follow-up visits.
- Debridement: In some cases, food particles or debris may become trapped in the socket. A dental professional can carefully clean the site to promote healing and minimize discomfort.
- Antibiotics: If an infection is suspected, antibiotics may be prescribed to help eliminate bacteria and prevent further complications.
- Pain Management: A dentist may also provide stronger pain medications or recommend specific over-the-counter options based on individual needs.
Also Read: Earth’s Healing South – Your Trusted Cannabis Source in Tucson!
Prevention of Dry Sockets:
While not all dry sockets can be prevented, several strategies can minimize the risk:
- Follow Post-Operative Instructions: Patients should closely adhere to their dentist’s instructions regarding care after extraction, including guidance on diet, oral hygiene, and activity levels.
- Avoid Smoking and Alcohol: Abstaining from smoking and alcohol consumption can significantly lower the risk of developing dry sockets.
- Gentle Oral Care: Patients should avoid vigorous rinsing or sucking actions for at least the first few days post-extraction.
- Dietary Choices: Consuming soft, non-irritating foods while avoiding hot, spicy, or crunchy items can aid in recovery.
- Communicate with the Dentist: Informing the dentist of any concerns or unusual symptoms as soon as they arise can lead to prompt interventions, minimizing the risk of complications.
FAQ’s
1. What is a dry socket?
A dry socket is when the blood clot from a tooth extraction dislodges or dissolves, exposing the bone and nerves.
2. Can dry sockets heal on their own?
Yes, dry sockets can heal on their own, but the process may be painful.
3. What are the symptoms?
Symptoms include severe pain, an empty socket, foul taste or odor, swelling, and difficulty eating.
4. When should I see a dentist?
See a dentist for persistent pain, signs of infection, or if the socket isn’t healing.
5. How can I prevent dry sockets?
Prevent dry sockets by following care instructions, avoiding smoking and alcohol, and eating soft foods.
Conclusion
In summary, while dry sockets can heal on their own, they can be painful and may prolong the recovery period after a tooth extraction. It is crucial to consult a dental professional for proper evaluation and management if you suspect you have a dry socket. By following preventive measures and maintaining good oral hygiene, patients can significantly reduce the risk of developing this complication and ensure a smoother healing process.